I see things like this: “Ataxia can strike anyone at any time regardless of age, gender, or race.” Misleading expressions like this are common for ataxia—blurring the lines between spinocerebellar ataxia (SCA) and other ataxia forms—and Huntington’s disease (HD).
This line of reasoning is ridiculous for dominantly inherited genetic diseases such as SCA and HD. It relies on fear mongering—i.e., questioning: do you really know the medical histories of your biological parents? Your four biological grandparents? Your biological aunts, uncles, nieces, nephews, and cousins? What about all eight of your biological great-grandparents and their descendants? And so on. Any one of them might have or have had a genetic disorder that you could be at risk of having, too.
Yes, this is on the outer fringes of being true, but only if you have no knowledge of at least one of your adjoining biological generations, such as if an entire branch of your family tree was wiped out at an early age. It’s much more likely that your family has lived for generations with genetic disease, and ideally many now would be using IVF + PGD or related technique (but I realize most aren’t) to avoid passing on the defect.
You can’t inherit an autosomal dominant genetic defect from anyone but one of your biological parents. If your parents didn’t have it, then neither do you, even if a grandparent did. But if you don’t know the medical histories of your biological kin, or if their presence was cut short without understanding their genetic situations, then things become sketchy. But being completely in the dark across generations is a rare corner case; saying that it applies to everyone in the world is recklessly disgraceful.
This seems to be part of an effort to de-rarify rare disease, in the name of support for those with the disease, to make them feel less alone. “Anyone could have what you have! Don’t you feel better now?”
What does it mean to be at risk of inheriting a specific autosomal dominant genetic defect?
Being at risk of inheriting a specific autosomal dominant genetic defect means that the defect is known to run in your family, yet you are asymptomatic and don’t know your genetic reality. Being genetically tested (assuming definitive test results) replaces risk (50%, or less) with certainty (either 0% or 100% risk). PGD is genetic testing at the fertilization stage that can eliminate genetic risk entirely.
What does “run in your family” mean? It means there’s an indication of the defect and/or disease among your biological: parents, aunts, uncles, nieces, nephews, cousins, grandparents, etc. You cannot get the defect from anyone but your parents, of course, but your parents’ situations might not be well understood. For a cousin to have it before you and your at-risk parent implies a biological aunt or biological uncle has/had it from the same biological grandparent that put one of your biological parents at risk—and, therefore, you.
Risk is there only if certainty isn’t. Certainty via genetic testing (post-birth or in an IVF dish) replaces risk; if done in the IVF dish, risk is reduced to 0% rather than the possibility of increasing it to 100% by testing post-birth.
Assuming no IVF + PGD, the risk of inheriting a dominant genetic defect from one generation to the next drops by 50%, meaning 50% of the parents’ conception outcomes results in an affected child. People can have their reality assessed (i.e., their at-risk number changed to 0% or 100% post-birth) by being genetically tested, assuming definitive test results.
Again, assuming no IVF + PGD, a child’s risk is half that of the parent’s risk. For example, if a parent’s risk is 50%, then the child’s risk is 25%. If the parent’s risk is ever “upgraded” to positive certainty, then any existing children’s risk jumps to 50%. If the parent’s risk is “downgraded” to negative certainty, then any existing children’s risk is eliminated.
At conception (assuming no IVF + PGD):
- 0% at-risk parent stays at 0% at-risk in children.
- 100% at-risk parent goes to 50% at-risk in children.
- Conception possibilities that result in passing the defect: 2 of 4.
- 50% at-risk parent goes to 25% at-risk in children.
- Conception possibilities that result in passing the defect: 4 of 16.
- 25% at-risk parent goes to 12.5% at-risk in children.
- Conception possibilities that result in passing the defect: 8 of 64.
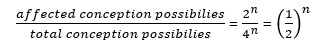
- More generally:
Risk can be eliminated across one generation using IVF + PGD, in which case the parent (i.e., not someone higher in the ancestral chain) needs to have a positive genetic test (100% at-risk).
In practice, above-0% risk probably never drops below 25% to 12.5%, because someone at-risk in the family tree will become symptomatic or tested, increasing risk elsewhere. Dominant defects typically cause adult-onset diseases, meaning at-risk parents can wittingly or unwittingly have half-as-at-risk children, but it’s unlikely that you would become a grandparent of at-risk grandchildren and not see the disease anywhere in your entire family (beginning with yourself).
Risk assessment is based on unknowns, not reality—i.e., not on the known presence or absence of the defect. Reality is whatever reality turns out to have been all along (0% or 100%); risk is somewhere in-between when reality is unknown. The well-known 50% chance (2 of 4) of inheritance across generations is a risk assessment and not a reality assessment. Only a genetic test can reveal reality, though becoming symptomatic was sometimes good enough before genetic testing, assuming a family history.
More risky examples
(All of these examples assume IVF + PGD aren’t used.)
If you know a parent has or had the genetic defect (100% at-risk, meaning “certain”), you and any siblings by that parent each has a 50% chance of being conceived with the same genetic defect. Put another way: if a parent certainly had it, but you don’t know if you have inherited it, you are 50% at risk of having inherited it. Genetic testing can replace risk with certainty. If you have your genetic reality assessed, either you’ll have the defect (100% at-risk) or not (0% at-risk).
Let’s say that your biological family’s medical history is unknown. Let’s say you had an affected parent, no one knew it, and that parent died or exited your life in some other way before becoming symptomatic or accurately diagnosed. You and any siblings by or of the affected parent (by the same affected grandparent), including descendants, don’t know it but all are at-risk of having inherited the defect.
If a grandparent is thought or confirmed to have (e.g.) HD, and yet you, your descendants, your at-risk parent, the siblings by or of your at-risk parent, including their descendants, all have an unknown status (i.e., asymptomatic and no genetic test), all are at risk of having inherited HD.
Let’s say that your biological family’s medical history beyond your grandparents is largely unknown or inaccurate. Let’s say you had a grandparent with (e.g.) HD, no one knew it, and that grandparent died before becoming symptomatic or at least before receiving an accurate diagnosis. As an alternative starting point, let’s say you had or have a grandparent misdiagnosed with a nongenetic disease, but that grandparent actually had or has a disease from an autosomal dominant defect. Let’s further say that your at-risk parent is not symptomatic and neither are you, any descendants of you, or any siblings by or of the at-risk parent, including their descendants. All don’t know it but are at risk of inheriting the defect from your grandparent.
The nonsensical example
Let’s look at the most egregious example of abusing at-risk numbers that I know of, which is the flagrantly specious at-risk number of 200,000 in the U.S. published many times with respect to Huntington’s disease.
https://rarediseases.org/rare-diseases/huntingtons-disease/
“About 30,000 people in the United States have Huntington’s disease and another 200,000 are at risk of developing the condition.”
This is deplorable nonsense of the highest order. It’s already known that there’s an upper maximum in the U.S. of about 30,000 with HD. Many of those people (especially young children) are untested and don’t know they are positive, but we have a statistical approximation of how many (total) there are.
It is simply impossible to have a large, additional group of at-risk people waiting in the wings to spontaneously sprout the disease. The number is not 200,000; it is zero. All corner cases are already wrapped up in the 30,000 number.
Leave a Reply